A colloid cyst is a non-malignant tumor in the brain. It consists of a gelatinous material contained within a membrane of epithelial tissue. It is almost always found just posterior to the foramen of Monro in the anterior aspect of the third ventricle, originating from the roof of the ventricle. Because of its location, it can cause obstructive hydrocephalus and increased intracranial pressure. Colloid cysts represent 0.5–1.0% of intracranial tumors.[1]
| Colloid cyst | |
|---|---|
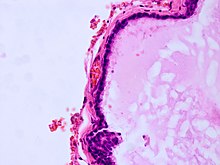 | |
| Histopathology of colloid cyst |

Symptoms can include headache, vertigo, memory deficits, diplopia, behavioral disturbances, and in extreme cases, sudden death. Intermittency of symptoms is characteristic of this lesion.[2] Untreated pressure caused by these cysts can result in brain herniation.[3] Colloid cyst symptoms have been associated with four variables: cyst size, cyst imaging characteristics, ventricular size, and patient age. Their developmental origin is unclear, though they may be of endodermal origin, which would explain the mucin-producing, ciliated cell type. These cysts can be surgically resected, and opinion is divided about the advisability of this.
Symptoms
editPatients with third-ventricular colloid cysts become symptomatic when the tumor enlarges rapidly, causing cerebrospinal fluid (CSF) obstruction, ventriculomegaly, and increased intracranial pressure. Some cysts enlarge more gradually, however, allowing the patient to accommodate the enlarging mass without disruption of CSF flow, and the patient remains asymptomatic. In these cases, if the cyst stops growing, the patient can maintain a steady state between CSF production and absorption and may not require neurosurgical intervention.[4]
Diagnosis
editColloid cysts can be diagnosed by symptoms presented. Additional testing is required and the colloid cyst symptoms can resemble those of other diseases. MRI and CT scans are often used to confirm diagnosis.[5]
Treatment
editThere are various management options depending on the severity of symptoms and their effects on the patient. The main management options are observation, craniotomy for microsurgical resection, neuroendoscopic removal, stereotactic drainage, and CSF diversion with bilateral ventriculoperitoneal shunting placement.[6][7]
Surgical resection
editMultiple studies have discussed how to remove a colloid cyst. One option is an endoscopic removal. An endoscope is inserted into the brain via a small incision and then moved toward the tumor in the ventricular compartment. The tumor is hit with an electric current. The interior of the cyst is removed followed by the cyst wall. The electric current is then used to kill the remaining pieces of the cyst. This whole process, including closing of the incision and removal of the scope, is completed within 45 minutes to an hour. The patients are able to leave the hospital after 1 or 2 days.[8] Quality of life is found to be better following endoscopic excision than microsurgery, with cysts smaller than 18 mm showing better cognitive outcome.[9] Another study found that ventriculomegaly may not be a contraindication for endoscopic removal, as the condition has comparable complication rates.[10] Another study experimented with a smaller retractor tube, 12 mm instead of 16–22 mm. The surgery was successful in removing the cyst; the smaller retractor tube minimized resection injury.
Neuroendoscopic third ventriculostomy during surgery can be used to prevent further postoperative hydrocephalus. This removes the need for insertion of bilateral shunts.[6][7]
Patients who have had a colloid cyst removed from the third ventricle sometimes experience some difficulty with day‐to‐day memory. Mammillary body atrophy in patients with surgical removal of colloid cysts indicates that this atrophy is partly due to a loss of temporal lobe projections in the fornix.[11]
References
edit- ^ Peeters, Sophie M.; Daou, Badih; Jabbour, Pascal; Ladoux, Alexandre; Abi Lahoud, Georges (1 June 2016). "Spontaneous Regression of a Third Ventricle Colloid Cyst". World Neurosurgery. 90: 704.e19–22. doi:10.1016/j.wneu.2016.02.116. ISSN 1878-8769. PMID 26968449.
- ^ Shaktawat, Sameer S; Salman, Walid D; Twaij, Zuhair; Al-Dawoud, Abdul (25 July 2006). "Unexpected death after headache due to a colloid cyst of the third ventricle". World Journal of Surgical Oncology. 4: 47. doi:10.1186/1477-7819-4-47. ISSN 1477-7819. PMC 1550234. PMID 16867192.
- ^ Schiff, David. "Cysts" (PDF). American Brain Tumor Association. Archived from the original (PDF) on 16 May 2017. Retrieved 26 October 2014.
- ^ Pollock, Bruce E.; Schreiner, Shawn A.; Huston, John III (May 2000). "A Theory on the Natural History of Colloid Cysts of the Third Ventricle". Neurosurgery. 46 (5): 1077–83, discussion 1081–3. doi:10.1097/00006123-200005000-00010. PMID 10807239.
- ^ Turillazzi, Emanuela; Bello, Stefania; Neri, Margherita; Riezzo, Irene; Fineschi, Vittorio (1 January 2012). "Colloid cyst of the third ventricle, hypothalamus, and heart: a dangerous link for sudden death". Diagnostic Pathology. 7: 144. doi:10.1186/1746-1596-7-144. ISSN 1746-1596. PMC 3502434. PMID 23078815.
- ^ a b Hadjipanayis, Costas G.; Schuette, Albert J.; Nicholas, Boulis; Charlie, Hao; Daniel L., Barrow; Charlie, Teo (July 2010). "Full Scope of Options". Neurosurgery. 67 (1): 197–205. doi:10.1227/01.neu.0000370602.15820.e4. PMC 2888508. PMID 20559107.
- ^ a b Garegnani, Luis; Franco, Juan VA; Ciapponi, Agustín; Garrote, Virginia; Vietto, Valeria; Portillo Medina, Santiago Adalberto (16 June 2020). "Ventriculo-peritoneal shunting devices for hydrocephalus". Cochrane Database of Systematic Reviews. 2020 (6): CD012726. doi:10.1002/14651858.cd012726.pub2. ISSN 1465-1858. PMC 7388891. PMID 32542676.
- ^ Colloid Cyst – New York Presbyterian Hospital Archived 22 June 2015 at the Wayback Machine. Nyp.org. Retrieved on 2013-08-15.
- ^ Dhandapani, S (1 October 2021). "Colloid cysts: Neuropsychological outcome, quality of life and long-term control after endoscopic gross total resection". Clin Neurol Neurosurg. 209: 106951. doi:10.1016/j.clineuro.2021.106951. PMID 34547641. S2CID 237524281.
- ^ Wait, S. D.; Gazzeri, R.; Wilson, D. A.; Abla, A. A.; Nakaji, P.; Teo, C. (2013). "Endoscopic Colloid Cyst Resection in the Absence of Ventriculomegaly". Operative Neurosurgery. 73 (1 Suppl Operative): ons39–ons47. doi:10.1227/NEU.0b013e3182870980. PMID 23334281. S2CID 6383791.
- ^ Denby, C. E.; Vann, S. D.; Tsivilis, D.; Aggleton, J. P.; Montaldi, D.; Roberts, N.; Mayes, A. R. (1 April 2009). "The Frequency and Extent of Mammillary Body Atrophy Associated with Surgical Removal of a Colloid Cyst". American Journal of Neuroradiology. 30 (4): 736–743. doi:10.3174/ajnr.A1424. ISSN 0195-6108. PMC 7051749. PMID 19164441.
Further reading
edit- Hamlat, A.; Casallo-Quiliano, C.; Saikali, S.; Adn, M.; Brassier, G. (2004). "Huge colloid cyst: Case report and review of unusual forms". Acta Neurochirurgica. 146 (4): 397–401, discussion 401. doi:10.1007/s00701-004-0221-8. PMID 15057535. S2CID 21210149.
- Beems, Tjemme; Menovsky, Tomas; Lammens, M. (2006). "Hemorrhagic colloid cyst". Surgical Neurology. 65 (1): 84–6. doi:10.1016/j.surneu.2005.03.034. PMID 16378869.
- Spears, Roderick C. (2004). "Colloid cyst headache". Current Pain and Headache Reports. 8 (4): 297–300. doi:10.1007/s11916-004-0011-2. PMID 15228889. S2CID 37231525.
- Benoiton L.A.; Correia J.; Kamat A.S.; Wickremesekera A. (2014). "Familial colloid cyst". Journal of Clinical Neuroscience. 21 (3): 533–535. doi:10.1016/j.jocn.2013.08.012. PMID 24308955. S2CID 206317368.
- Melbourne Neurosurgery