Sleepwalking: Half-Asleep But on the Move
Sleepwalking: Half-Asleep But on the Move
By Antonio Zadra, PhD
That people sometimes engage in complex behaviors during sleep has been known for centuries. As an example, Shakespeare’s Macbeth contains a widely known episode of sleepwalking (also known as somnambulism), during which a guilt-ridden Lady Macbeth tries to wash imaginary bloodstains from her hands while speaking of the crimes she and her husband have committed.
But what, exactly, is sleepwalking? The symptoms that characterize this unusual and at times dramatic sleep disorder can vary greatly across affected individuals; even in the same person, the symptoms may vary from one episode to the next. Episodes can be mundane and stereotyped, such as sitting up in bed, pointing at a wall, fingering bed sheets, and walking about a room, or they can be surprisingly complex, such as rearranging furniture, cooking, getting dressed, or playing a musical instrument. Consequently, episodes may last from a few seconds to a few dozen minutes. Sleepwalkers typically have their eyes open throughout an episode and, contrary to common depictions of the disorder, do not move about with their arms stretched out before them!
Whereas most children do not remember their sleepwalking episodes, it is not unusual for adult sleepwalkers to remember perceptual, cognitive, emotional, or behavioral aspects of their episodes. In fact, recent sleep lab studies have also shown that complex “dream-like” experiences can play a role in the behaviors exhibited during sleepwalking. It should be noted, however, that whereas sleepwalkers are aware of their immediate physical environment during an episode and can interact with other people nearby, this is not the case in normal dreaming. Also, sleepwalking arises out of deep, slow-wave sleep, and never out of rapid eye moment (REM) sleep, the sleep stage most strongly associated with vivid dreaming.
S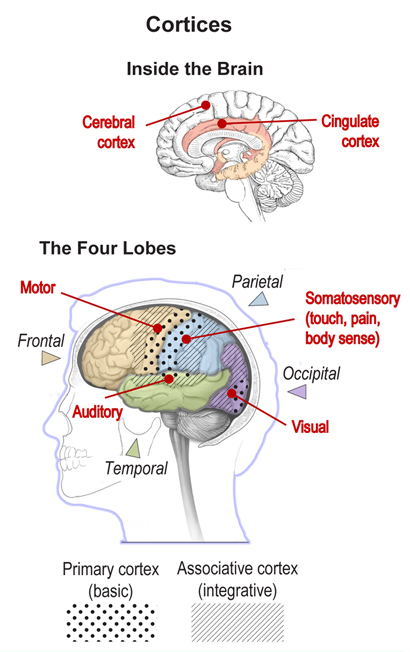 leepwalking is more common in childhood than in adulthood, but childhood somnambulism is typically benign (and nonviolent) and usually does not require any intervention. The peak incidence of sleepwalking (approximately 29% of children sleepwalk) appears around 11 to 12 years of age, before rapidly decreasing during adolescence. Sleepwalking affects 2% to 4% of the general adult population, and is associated with considerable harm potential, including placing oneself in dangerous situations (for example, running into walls and furniture, trying to escape imaginary threats, leaving one’s house), destroying property, and having episodes result in serious injuries to the sleeper, bed partner, or others. In fact, a history of aggressive and/or injurious behavior during sleep is what leads a strong majority of adult sleepwalkers to consult a medical specialist.
leepwalking is more common in childhood than in adulthood, but childhood somnambulism is typically benign (and nonviolent) and usually does not require any intervention. The peak incidence of sleepwalking (approximately 29% of children sleepwalk) appears around 11 to 12 years of age, before rapidly decreasing during adolescence. Sleepwalking affects 2% to 4% of the general adult population, and is associated with considerable harm potential, including placing oneself in dangerous situations (for example, running into walls and furniture, trying to escape imaginary threats, leaving one’s house), destroying property, and having episodes result in serious injuries to the sleeper, bed partner, or others. In fact, a history of aggressive and/or injurious behavior during sleep is what leads a strong majority of adult sleepwalkers to consult a medical specialist.
Among the general factors known to contribute to the occurrence of sleepwalking, genetics appears to play a key role. About 80% of somnambulistic patients have at least one family member affected by this disorder, and the prevalence of somnambulism is higher in children of parents with a history of sleepwalking. One study of more than 300 pairs of twins found that monozygotic (identical) twins are concordant for the disorder six times as often as dizygotic (nonidentical) twins.
We now know that during somnambulistic episodes, some regions of the sleepwalker’s brain are awake while others are still fast asleep. The sleeping parts include the associative cortices, which help us integrate visual, auditory, and other sensory stimuli into our conscious experience; their deactivation is typical of sleep. At the same time, networks in the motor cortex and – in the limbic system deeper in the brain – the cingulate cortex are activated; that’s typical not of sleep but of emotionally guided motor behavior (movement) during wakefulness. It is this coexistence of deep sleep and wakefulness that explains the unusual mental state in which sleepwalkers find themselves.
Treatment for sleepwalking is unnecessary when the episodes are benign and not associated with potential injury. In this case, reassuring the patient and his or her family about the benign nature of the episodes and demystifying the events is often sufficient. In addition, while stressors can precipitate sleepwalking in predisposed individuals, it is important to note that sleepwalking is not a sign of deep-seated anxiety or other forms of mental illness. However, attention should be paid to potential precipitating factors, such as sleep deprivation, stress, and environmental disturbances that may fragment sleep, so that such factors can be avoided.
For patients with a history of more agitated, less benign somnambulism, precautions should be taken to ensure a safe sleep environment. Preventative measures can include the removal of obstructions in the bedroom, securing windows, arranging for the sleepwalker to sleep on the ground floor, installing locks or alarms on outside doors, covering windows with heavy curtains, using a nightlight, placing barriers in stairways, and removing all sharp or otherwise dangerous objects.
Controlled clinical trials for the treatment of somnambulism are lacking. Hypnosis (including self-hypnosis) has been found to be effective in both children and adults presenting with chronic sleepwalking. Relaxation exercises, such as autogenic training or progressive muscle relaxation, if carried out regularly before bedtime, can also help decrease the number of episodes.
In children, the preferred treatment for somnambulism consists of a behavioral technique called anticipatory or scheduled awakening. Parents keep a diary of their child’s episodes and determine the approximate time at which the episodes typically occur. They will then awaken their child about 15 to 20 minutes before the episode’s typical time of occurrence, every day for one month. This simple intervention can yield rapid and lasting results, possibly by reducing a build-up of deep sleep early in the night, a condition that can give rise to episodes in predisposed children.
Sleepwalking in adults can also be triggered by a primary sleep disorder such as sleep apnea. In these cases, treatment of the primary sleep disorder often results in the alleviation of sleepwalking.
Pharmacological treatments, such as benzodiazepines, should be considered only if the behaviors are very frequent (every night or even several times a night), hazardous, or extremely disruptive to the bed partner or other household members. However, pharmacotherapy does not always result in adequate control of sleepwalking. It is recommended that treatment approaches always include instructions on sleep hygiene (habits that contribute to sleeping well), avoidance of sleep deprivation, and stress management.
…………………………………………………………………………………………………………………………..
© 2018 Antonio Zadra. Antonio Zadra, PhD, is a professor of psychology at the Université de Montréal (Canada) and director of the university’s Dream Laboratory. He leads a research group investigating non-REM sleep parasomnias at the Center for Advanced Research in Sleep Medicine. His research focuses on the relation between dream content and waking experiences, the correlates and treatment of dream-related disorders, and the pathophysiology of sleepwalking.
Banner images: (Center) From the Sleepwalking collection, Alex Bamford Photography. (Left) Plate 1. Sir Charles Bell, The anatomy of the brain, 1802. Wellcome Collection, CC BY.
The International Association for the Study of Dreams is a nonprofit, international, multidisciplinary organization dedicated to the pure and applied investigation of dreams and dreaming. Our members variously explore dreams through the sciences, the humanities, the arts, clinical applications, and their own experiences. See our website (ASDreams.org) for information on dream research, research grants, membership, and conferences. IASD is a partner in the global Brain Awareness Week campaign of the Dana Alliance, which offers a large selection of brain education materials on its website (dana.org/baw).